Editor’s note: Find the most recent COVID-19 news and assistance in Medscape’s Coronavirus Resource Center.
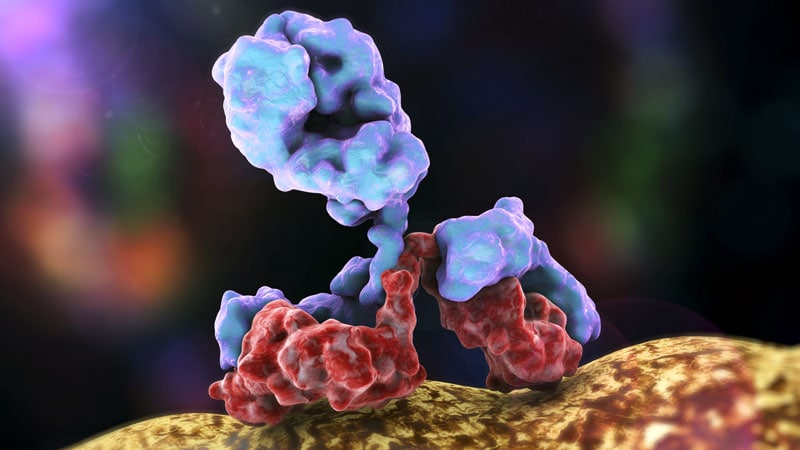
Monoclonal antibodies (mAbs) to deal with COVID-19 remain in sufficient supply, however little proof on their efficiency, paltry repayment, and an absence of a planned infrastructure to administer them has actually resulted in significant underutilization of these potentially useful treatments, according to a brand-new report from The National Academies of Sciences, Engineering, and Medication.
The 35- page report described missed chances to work with states and health centers to develop trust with clinicians and patients, and to establish an infusion facilities to funnel patients to websites. Though the therapies still require more research study, they should be an option for the ideal client at the right time, stated the National Academies specialists in their report, Rapid Specialist Assessment on Designating COVID-19 Monoclonal Antibody Treatments and Other Unique Rehabs
” No potentially qualified patient must be left uninformed, and no qualified client ought to be denied access, if there are doses readily available and the patient and doctor concur it is a reasonable course,” they concluded. The report likewise kept in mind that underuse, and in specific underuse by members of vulnerable and underserved neighborhoods “raises issues about exacerbating currently dramatic health disparities.”
The federal government has invested $375 million on Eli Lilly’s bamlanivimab and $450 million on Regeneron’s casirivimab plus imdevimab cocktail, and concurred last month to invest as much as $2.6 billion more on as much as 1.25 million extra doses.
Some 785,000 dosages of the two rehabs have actually been produced and about a half million have actually been distributed to states. But about three quarters have gone unused. The US Department of Health and Human being Providers has actually released an online treatment locator to attempt to stimulate interest in the therapies.
However the federal government hasn’t resolved a few of the fundamental barriers to use of the monoclonals, said the National Academies specialists.
” Absence of awareness, interest, and self-confidence in COVID-19 mAb therapies among patients and suppliers are major issues,” they said in the report. Patients who have tested favorable might not wish to take a trip to an infusion website, while others may not have access to healthcare, or only look for such treatments when it’s too late. Some who are qualified might not have the time, resources, or transportation to go to a website and endure a 2-hour treatment.
In addition, “the supply and availability of infusion centers and workers was determined as a greater restraint than the supply of COVID-19 mAbs,” said the report.
Expense a Huge Obstacle
.
While the federal government has actually covered the expense of the treatments, healthcare facilities and patients inevitably incur related costs.
” The fragmented payment system in the United States has actually not offered adequate support to cover the spectrum of expenses associated with COVID-19 mAb therapies,” stated the report. That is intensified by persistent underfunding and limitations on federally certified university hospital for neighborhood health, the report said.
Clients might have to spend for testing, office visits, follow-up consultations, transport to and from the infusion site, and potentially a copay for the administration of the drug.
While Medicare pays healthcare facilities $309 per infusion, that might not suffice, especially if a health center or other website had to construct out a brand-new infusion center, the report reveals. For clinicians, the administrative payment under Medicare Part B does “not cover the total practice cost to provide infusion services, leading to a significant cost-reimbursement disparity,” the report states.
In addition, there are no particular codes for observing patients throughout the 2-hour procedure.
” The established Medicare payment rate for providing COVID-19 mAb treatments does not cover the cost related to collaborating care for those clients, nor does it validate the risk and opportunity costs connected with purchasing facilities adjustments to safely incorporate COVID-19 clients into existing centers or constructing short-term infusion capability,” the report concluded.
More Information Required
.
The US Fda released emergency situation use authorizations (EUAs) for the two monoclonal treatments based on phase 2 trial information, and that leaves a lot of unpredictability, noted the National Academies.
In trials, both treatments reduced COVID-19- associated hospitalizations and emergency room check outs within 28 days after treatment amongst patients at high danger of development compared with those who got placebo.
However clinicians aren’t particular about who ought to use the monoclonals, stated the report. The underuse has in turn resulted in problem gathering information– either through continuous trials or in beginning brand-new trials.
The National Academies advised allocating the monoclonal antibodies in a way that would generate better information collection to inform clinicians. Payers might support the advancement of a core data platform or pc registry, or Medicare might develop pilot trials, stated the report.
Lilly and UnitedHealth Group are working together on a study in high-risk Medicare patients, according to Reuters Clients who evaluate positive will be given bamlanivimab in your home.
” Building infusion capability and developing the proof base about the impact of COVID-19 mAbs on medical results aside from hospitalization, including mortality, are the most promising techniques for increasing effective usage moving on,” specified the National Academies report.
For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube.
No comments:
Post a Comment