.
Monoclonal antibodies are laboratory-made particles that in this case simulate the body immune system reaction to SARS-CoV-2, targeting a particular part of the extending “spike” proteins on the surface area of the infection, avoiding it from binding to cells or tagging it for damage. Scientist initially separate antibody-producing B cells from clients who have actually recuperated from COVID. They go on to discover the most powerful of these antibodies and after that produce them in mice crafted with parts of the human body immune system.
Making use of monoclonal antibodies for the treatment of COVID got nationwide and global attention last October, when President Trump got an antibody mixed drink made by Regeneron after he was identified with the health problem. Soon afterwards, 2 monoclonal substances got Emergency situation Usage Permission (EUA) by the U.S. FDA and were anticipated to be a crucial part of the reaction to the pandemic.
However a variety of aspects have actually restricted their usage. There has actually been an increase in more infectious SARS-CoV-2 variations, a few of which show reduced vulnerability to the monoclonal antibodies. Troubles have actually likewise occurred in administering these substances to outpatients with moderate and moderate illness in overloaded medical facilities. The usage of these drugs can still slow illness in some clients who are at danger of aggravating, and they might likewise be beneficial in avoidance.
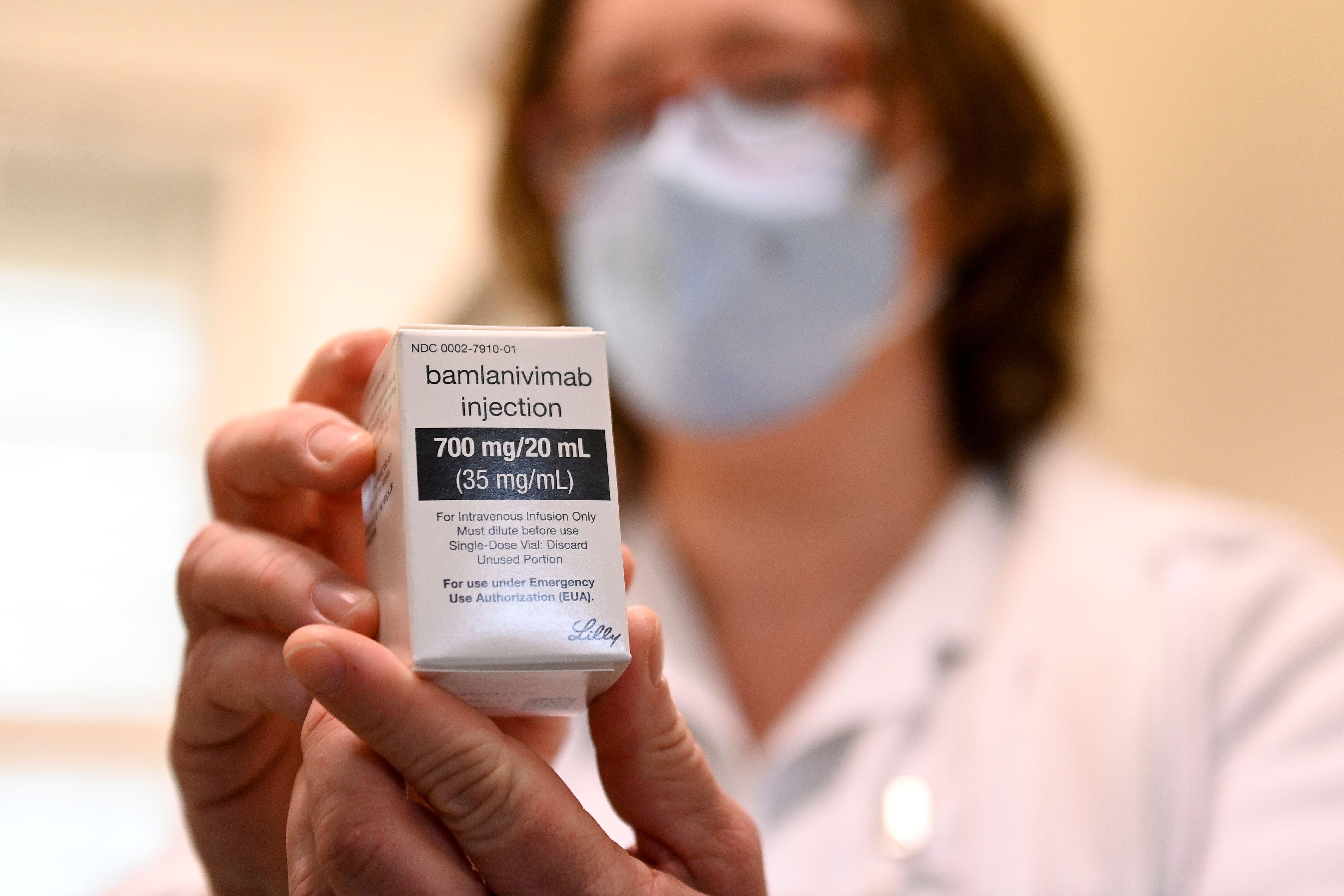
Today there are numerous monoclonal antibodies that have actually been studied and for which the FDA has actually provided EUA. This classification is not an official approval, however it lets drugs be utilized throughout public health crises. Drugs with EUAs at first consisted of bamlanivimab(likewise called LY-CoV555 and LY3819253), etesevimab (LY-CoV016 and LY3832479), casirivimab (formerly REGN10933) and imdevimab (formerly REGN10987). In November, the FDA approved an EUA for both bamlanivimab and, individually, the mix of casirivimab/imdevimab for usage in outpatients with moderate to moderate COVID who are at high threat of development to serious health problem.
These approvals were based upon an interim analysis of 2 mid-stage (stage II) medical research studies amongst outpatients with moderate to moderate COVID in which these substances appeared to speed up the decrease in viral load in a client. Since of a boost in the number of SARS-CoV-2 variations resistant to bamlanivimab (from around 5 percent in mid-January to 20 percent in mid-March 2021), the FDA withdrawed the EUA for bamlanivimab on April 16, 2021, and it is no longer readily available for usage as a sole treatment for clients. 2 items that integrate monoclonals (bamlanivimab plus etesevimab, or casirivimab plus imdevimab), are still readily available through an EUA for the treatment of moderate to moderate COVID in nonhospitalized clients at high danger of advancing to serious illness or hospitalization. None of these drugs have actually been revealed to be of advantage in sicker hospitalized clients.
Presently the NIH COVID treatment standards suggest that a person of the 2 mixed drinks be administered for the treatment of outpatients identified with moderate to moderate COVID infection who are at high danger of development to extreme illness. The treatment requirements consist of having a body mass index of 35 or more, being 65 or older, having diabetes, persistent kidney illness or an immunosuppressive illness, or taking an immunosuppressive drug. Some individuals more youthful than 65 are likewise qualified if they satisfy particular requirements. Information on making use of these drugs for clients more youthful than 18 years of ages are restricted.
When recommending these treatments, it is necessary that treatment be begun as quickly as possible after the medical diagnosis and within 10 days of start of signs. The Transmittable Illness Society of America standards note that the information are more powerful for bamlanivimab/etesevimab than for casirivimab/imdevimab. They likewise advise that prescribers take into account which variations are distributing in the neighborhood and whether or not they are prone to monoclonal treatments.
The rollout for monoclonals came just a little prior to the intro of extremely efficient vaccines. With the vaccines’ arrival, monoclonals have actually not been as commonly utilized as initially considered and are being scheduled for individuals who can not be immunized, those who do not react to the vaccine or individuals who require instant prophylaxis after a considerable direct exposure.
After President Trump was treated with monoclonals and after the FDA released its EUA, the federal government bought over 500,000 dosages of both bamlamivimab and casirivimav/imdevimab, anticipating high need for these drugs.
Not just was the need from clients weaker than forecasted however health centers and centers had a hard time to get these treatments to clients. There are numerous descriptions regarding why. Clients in some cases postpone looking for care up until more than 10 days after the start of signs. Test outcomes might lag. Logistical concerns emerge in administering an infusion or injection at a website where a client with COVID can be securely seen. Most likely the biggest barrier over the December-to-January duration was that health centers were overwhelmed with ill clients and just did not have the personnel to administer these drugs to clients that were “not ill enough.”
So, do I still believe these work drugs? Definitely. We are presently tape-recording around 60,000 brand-new infections daily in the U.S., and numerous are taking place amongst individuals who would gain from monoclonal antibody treatment to avoid development of COVID to extreme illness and hospitalization. The word about monoclonals still requires to go out. Regeneron, in reality, aired an ad throughout the 2021 Academy Awards, wishing to inform clients about the worth of these substances.
For monoclonals to be more commonly dispersed, the possibility of administering them subcutaneously or intramuscularly instead of intravenously need to be checked out. We ought to likewise move their administration from the center into drug stores and screening websites where it can be more quickly and easily done.
As long as we continue to have cases of COVID, vaccination ought to not be the only method we carry out for control. While development has actually been made immunizing high-risk populations in the U.S., we still require to increase access to reliable treatments that can avoid illness development, hospitalization and death amongst those who get contaminated with SARS-CoV-2.
This is a viewpoint and analysis post.
No comments:
Post a Comment